A Bendigo woman has become the first person to see Victoria’s voluntary assisted dying (VAD) laws through to their conclusion.
Kerry Robertson, 61, was the first person to receive a permit under Victoria’s new Voluntary Assisted Dying Act, visiting her doctor the day the law came into effect.
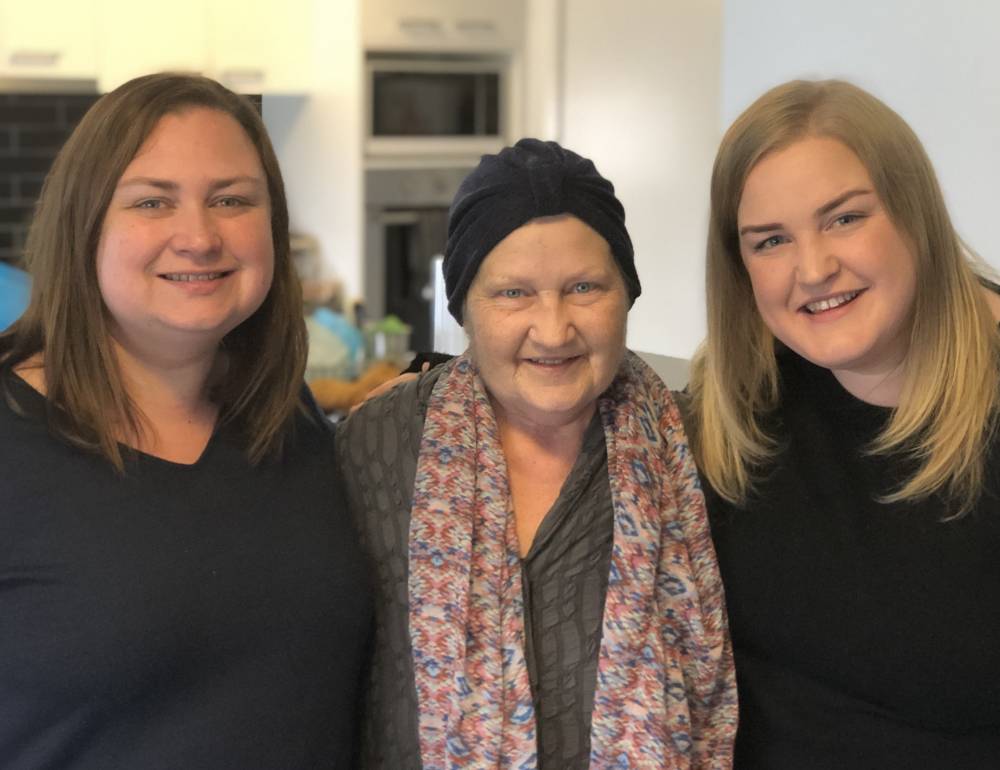
Ms Robertson’s daughters, Jacqui Hicks and Nicole Robertson, told Go Gentle their mother’s death was “beautiful and peaceful”.
Both daughters were with their mother when she died.
“It was a… positive experience. It was the empowered death that she wanted,” Ms Hicks said.

Ms Robertson was diagnosed with breast cancer in 2010. She underwent treatment, but her cancer spread to her bones, lungs and brain.
By March this year, the disease had spread to her liver. The chemotherapy Ms Robertson was receiving was causing unmanageable side effects.
Ms Robertson eventually made the difficult decision to stop all treatment.
When assisted dying became legal in July this year, Ms Robertson already had an appointment booked with her doctor. She made her first request to access a voluntary assisted death at that appointment.
“Mum already had an appointment booked to see her specialist the day the legislation came into effect, she made her first request that same day,” Nicole said.
The women said the assisted dying process went smoothly and took 26 days to complete. Ms Robertson took the medication the day it was dispensed by the state-wide pharmacy.
She died in a Bendigo nursing home on 15 July.
“It was quick, she was ready to go. Her body was failing her and she was in incredible pain. She’d been in pain for a long time,” Nicole said.
“Palliative care did their job as well as they could. But it had been a long battle. She was tired, the pain was intolerable and there was no quality of life left for her.”

Ms Hicks said her mother “left this world with courage and grace”.
“We were there with her; her favourite music was playing in the background, and she was surrounded by love.”
“We did everything we could to make her happy in life, and comfortable in death,” Nicole said.
Ms Robertson’s daughters told Go Gentle seeing their mother access the VAD laws reinforced their belief that anyone who has a terminal diagnosis, is suffering, and in intolerable pain should have the option to access a voluntary assisted death.
“It is the most compassionate, dignified and logical option for those suffering in the end stages of life,” said Nicole Robertson.
Go Gentle Australia’s director Andrew Denton said Ms Robertson’s experience demonstrates the effectiveness of the new law.
“The eligibility criteria were met, the safeguards were worked through, and Kerry Robertson and her family were offered the compassionate death Kerry wanted,” he said.
Mr Denton also noted that accessing the process was not difficult, even though the family lived in regional Victoria.

VAD laws were passed in Victoria’s parliament in 2017.
They are the most conservative of their type in the world. Patients must meet strict eligibility criteria to be considered for the process.
To be eligible, the person must be 18 years of age or older, and they must have lived in Victoria for at least 12 months.
They must have a terminal illness and expect to live no longer than six months, or 12 months if the person has a neurodegenerative disease such as motor neurone disease.
Those interested in accessing voluntary assisted dying must find a doctor with the appropriate qualifications to determine if they are ‘eligible’. A second doctor then also has to determine if the person is eligible.
If deemed eligible, the patient then has to put their request in writing, and at least nine days later, they must write a second request.
On receiving the final request, the doctor will apply for a permit to prescribe the medication that can be used to end the patient’s life.
Main image: (left to right) Jacqui Hicks, Kerry Robertson, and Nicole Robertson. Image: Go Gentle.