
The aged care industry, like other areas of the healthcare system reliant on health professionals, are facing major challenges in sustaining a healthy workforce to meet the rapidly rising demand in Australia’s ageing population. This is amongst a backdrop of many of the more acutely ill ageing population living in nursing homes now requiring more intensive levels of care such as post-operative care, palliative care and dementia with challenging behaviours.
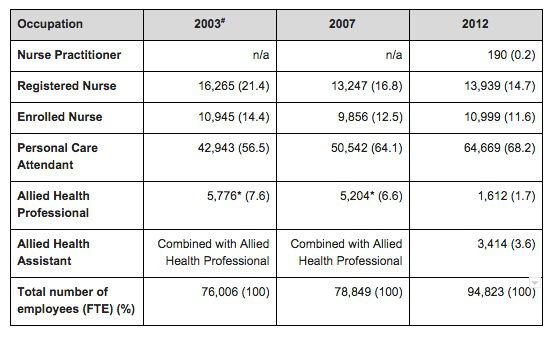
To set the scene, there are some 358,497 practicing registered nurses and midwives in Australia (2015) [Nurse & Midwife Registrant Data]. Importantly, however the last available national statistics on the aged care sector (Australian Government Department of Health and Ageing 2012, see table below) highlight a trend to increasing personal care attendants (PCA) and a slower growth, certainly not enough to keep up with the industry growth and demand for beds, of registered nurses (RN).
During the global financial crisis the number of nurses leaving the workforce declined, however it is expected to rise in the next few years as nurses explore greener pastures and consider new careers. The number of nurses and personal carers that leave the workforce is one third higher than for the health care and social assistance industry and slightly higher than for the economy in general. The Productivity Commission was of the view ‘that the sector overall has a high turnover rate, with around one in four personal carers having spent less than a year with their current employer’. High staff turnover isn’t only an expensive exercise for aged care providers, but also unsettling for residents in their care. The impact is often a reduction in the quality of care provided.
So why is staff turnover in aged care is so high? Over the years I have witnessed many skilled, passionate and dedicated senior and junior nurses, and personal carers, vacate the workforce. Either returning to the acute, exploring other areas of the healthcare industry, or simply wanting to leave the industry for good. While the reasons aged care workers may choose to leave the industry are multifactorial, in most cases it’s not because they no longer want to care for the elderly but for more emotive reasons that I will discuss in more detail shortly.
What is it about working in aged care that is compelling this mass exodus, or ‘brain drain’ so to speak from the sector, and how can we encourage and promote the positive aspects of working in aged care to young graduates, or experienced nurses alike? After all caring for the elderly and providing the very best care to them can be one of the most rewarding parts of the job where individuals can feel satisfaction in making a difference in the lives of others. A report published by The Department of Health elegantly summarises from my experience why aged care workers, in particular nurses are leaving the profession, some include:
A recent report indicating sector profits are increasing substantially for some aged care providers, showing 40 per cent up on last year, whilst the hours of care delivered to older people are reducing, down 7 per cent. In particular from trained nurses, and other costs per resident.
A 2012 report released by The Department of Health & Ageing, Aged Care Workforce, showed the disparity in average weekly earnings between aged care and acute care nurses is a $114 per week nationally, in favour of the acute care nurses. With the greatest disparity in the Northern Territory at $295 per week, it’s no wonder they struggle to attract nurses to the outback. Remuneration is symbolic of more than an employee’s pay packet, it’s symbolic of an employer’s recognition for their team’s hard work, appreciations and motivation, as well as their sense of ‘worth’. To be paid a low salary in combination with feeling unappreciated by the employers, quickly leads to an unmotivated workforce, not wanting to do more than the bare minimum and if they stay in their role, not emotionally connected or providing quality care. In more and more cases, this is leading to the staff seeking opportunity to ultimately exit the industry.
Having low paid, low skilled workers delivering care to people with chronic and complex conditions, severe dementia and behavioural disorders in many cases puts quality of care of these particularly vulnerable people at risk and will the problem only projected to get worse.
Often it’s not the actual day-to-day work that hastens nurses leaving a career in aged care, nor is it remuneration alone, with nurses aware of the salary before entering the profession in the first place. However when you couple working conditions, lack of professional development and leadership among the other areas mentioned, at some point, it gets the better of the individual that had expected more.
Leadership education for nurses, or the lack thereof is also suggested as a reason for turnover with good clinical nurses at some point promoted into leadership roles without the qualification, skills or mentorship to undertake this important role of not only motivating and inspiring a team, but also ensuring the delivery of quality care to residents. Without seeing the need for development, or simply failing to invest in nursing care expertise in the first place, has a multitude of economic and social impacts too. Nursing as a profession is one of the largest health professions, working in most areas that healthcare is delivered. No other health professional group offers the same capacity and reach for health care delivery as nurses.
Difficult working conditions including insufficient time to complete the necessary requirements for each resident being supported by a nurse in the facility to ensure they are provided with quality care, too often gets the better of nurses with a particularly high personal standard. Job satisfaction, quite understandably among nurses is closely related to having adequate opportunities to provide quality care and team collaboration. If nurses are unable to maintain care standards and continue to be excellent clinicians, as their workloads increase along with their scope of practice, preventing them from providing humane and holistic care, then it’s no wonder good nurses reach a tipping point and leave. Competent and skilled nurses play a critical role in ensuring a high standard of clinical care and leadership are delivered. They are a critical link with other members of a resident’s multidisciplinary team often responsible for observing health issues in a resident earlier than a doctor may have opportunity to see a concerning symptom. They are part of the ecosystem of care and support that the health system cannot operate without and relies on for efficiency in early identification, and prevention. Without nurses the workforce and sadly our elderly under their care suffer as a result.
It is common for nurses to work long hours, in some cases unpaid overtime or working without breaks, just to ensure the basic standards of care are delivered. Work related stress, can stem from the sheer workload and significant responsibility of overseeing the care of residents’ needs. Coupled with managing the high standards and expectations of residents, or the questions and demands of their concerned families and guardians (and rightly so I must add). This can be a challenging aspect of the job, especially when some nursing and personal carer staff have not received adequate interpersonal training to do this; to listen to the family, understand and acknowledge their concerns and provide reasonable and transparent information, and expectation management, fairly and sensitivity for the situation the loved one of the family may be facing. This is made even harder when at times as a nurse, you may in fact completely agree with the family that is raising a particular concern or complaining however, how does one explain to them that as a nurse operating in today’s environment with today’s pressured time conditions and limited support staffing resources, that nurses simply do not have the bandwidth to complete some requested or missed tasks as trivial or important as they maybe; or a nurse simply can’t guarantee staff will think to action a family’s request or a resident’s requirement every day with the level of care delivery being so person dependent. None of these scenarios being a reasonable outcome under the lens of quality of care.
Lack of management action and the behaviour of some managers was identified in the report by The Department of Health & Ageing as a highly significant factor impacting on employee turnover in the nursing profession. Nursing leaders themselves confirmed that within the overall culture in healthcare services, work conditions across Australia need to improve and organisations need to evolve their standard practices by developing supportive and strong leadership to drive collaborative and supportive action sustainably amongst the workforce against the backdrop of staff turnover. This is necessary for organisations to enhance contemporary clinical practices as well as improve the environment overall staff job satisfaction and working conditions.
In the absence of effective leadership, employee satisfaction can be affected, along with trust in management, the culture of the organisation, the individual’s commitment to do more than the basic requirements, and individual and team effectiveness in general. Leadership is central to mobilising individuals and teams towards a common goal, creating a positive working environment that is successful in attracting and retaining a high standard of nursing staff, as well as achieving outstanding health outcomes. Given the issues faced by the sector, the leadership in the nursing sector and those responsible for it have a large burden and challenge ahead of them indeed.
There remain a number of areas of the aged care workforce and systemic issues in the sector that need to be addressed at both an industry level and within individual organisations to put a halt to the ‘brain drain’ effect that sees many skilled and passionate nurses leaving the industry. ‘Brain Drain’ is a term often used to reflect the loss of talent and experience from Australia to overseas markets but in this case it is the loss of competency, experience and qualification form a sector, the aged care nursing sector, and the issue is only getting worse.
Major issues around workplace environment and the culture embedded in practices for some individual nursing homes and organisations alike are a direct result of the lack of management and leadership skills present, along with levels of remuneration and workloads for aged care workers. Whilst some of the areas talked about around job dissatisfaction are intrinsic to the nature of the work, some others may easily be addressed, mitigated and improved by the actions of management. Strategies will need to include creating a culture of supporting one another, showing staff they are appreciated for what can be an often thankless job, developing and investing in the training of skilled clinical staff to take the next step as a leader in management, leadership to not only support the workforce but continue the focus on improving and ensuring excellence in the delivery of care to residents. The ability to perform one’s job well often directly results in a more cohesive and satisfied workforce, and critically, helps ensure the quality of care for patients, residents and loved one’s in their care.
I did not realise but burn out was occurring with me and I should have been able to seek some help. Instead I carried on and then called it a day. I was just too concerned about the amount of medications being prescribed and the idea of crushing so many. Many clients would refuse them but the prescribers would not stop them even though it was obvious on the medication chart, it was refused. I felt that a lot more could be done regarding medications by reviewing them with trials without them and more client and family reviews. I saw people with PEG tubes who obviously did not want them, continually pulling them out (they were very clear of mind) only to have them being replaced time after time. A person may have been prescribed 10 medications while having a PEG tube and these drugs should be crushed and given singularly. I could not come to terms with the amount of medication.
Lauren thorouhly enjoyed reading this article it is exactly how our unit feels and we could add a lot more by several incidents that have happened with valuable young nurses furthering their eduction but completely refusing any guidance or support from management re study leave or rotating to other acute areas to put into clinical practices what they are studying at uni so unfortunately they have left to have better flexiabliity while studying and working shift work . We lost 3 junior nurse who were so great in aged care but were encouraged by senior nurses to further themselves whilst so young which they enrolled to do but were not encouraged by management why?As we all agreed that hopefully these staff with education clinical experience and general life skills within nursing would return themselves as managers num or in some admin capacity in aged care as they loved the culture and care of the elderly. I personally have nursed since 1976 and loved and learnt in all areas I have been but I have in aged care since 1994 and still enjoy my work but get extremely disilliuled by the uninterested managers that have no idea and would not know one resident to another yet can sit in handoverand tell staff that mr or Mrs are only making said dollar amount and staff need to bring that dollar amount up , staff respect funding but do not need to be told this especially at handover .Lauren I could go on and on but extreme thanks for your articles they are very consoling and encouraging to keep the valued staff to look after very valued people.